Limb Reconstruction and Coping with External Fixation
Limb Reconstruction is a term widely used to describe the acute or slow correction of angular or length deformities in bones. In many cases a complete correction can be performed at a single surgery. The correction may be a gradual process, which lengthens and/or straightens bone and soft tissue so a limb can function as normally as possible. There are many reasons why someone may be a candidate for limb correction, including past trauma, which resulted in highly fragmented breaks, infection, arthritis, bone loss or a non-union (a fracture that is not healing). Dr. Mackie sees many patients through his Royal Hobart Hospital commitments with deformities from birth defects or related to bone growth damage during childhood.
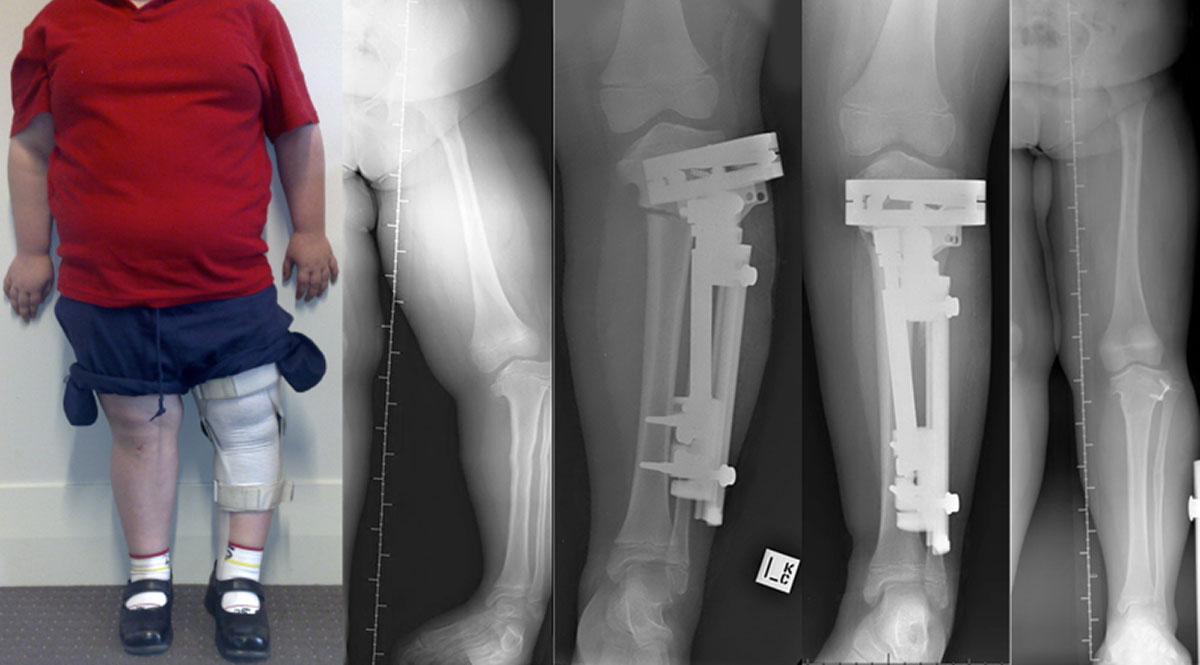
Acute Bone Correction for Angular Deformity
Provided there is little risk to other structures a misaligned bone may be cut, realigned and then the bone may be stabilised with various options including wires, screws, metal plates, external frames. Correction can be performed close to a joint in skeletally mature patients (growth plates have finished their growth at around age 17 for males and around 15 for females). If single stage surgical correction is performed in skeletally immature patients then techniques may need to be used to try and avoid operating close to growth plate.
Acute bone corrections have the advantage of completing the positioning of the bone in one surgical step and then allowing healing to occur. Some deformities are too significant to safely correct in this manner because of the stress or tension placed on surrounding tissues / structures.
Guided Growth Deformity Correction
This is only suitable for growing bones with a growth plate which can have its rate of growth modulated or altered with surgery. The timing for surgical intervention is determined by the magnitude of the deformity and the anticipated amount of growth left in the limb. Part of the growth plate may be stopped or slowed in its growth to allow the remaining growth plate to “drive” the correction of the deformity. “Epiphysiodesis” is a term from the Greek in which "physis" means growth plate and "desis" means tether. By tethering one side of a growth plate the deformity is slowly corrected during ongoing growth. This process of growth may take many months to occur.
Slow External Fixation Deformity Correction
External fixation frames are orthopaedic surgical equipment, which allow stabilisation of bone and joint deformities or allow gradual correction of bone and joint deformities. External frames are generally used in circumstances when internal fixation (rods, plates, screws) cannot be utilised. The principles of slow deformity correction with external frames were advanced by a surgeon in 1950’s and 1960’s Russia (Dr. Gavriel Ilizarov). Many of the current techniques used for arm or leg deformity correction are termed “Ilizarov technique”.
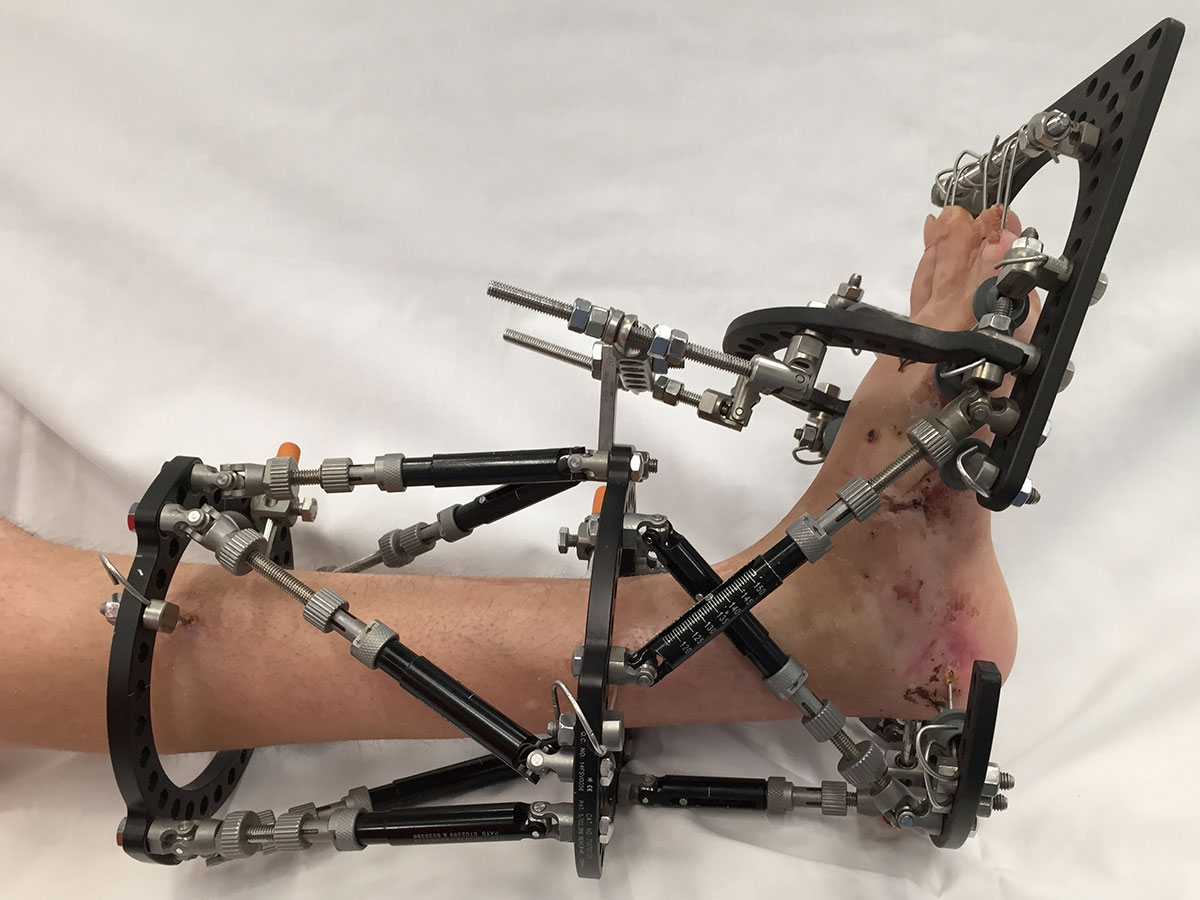
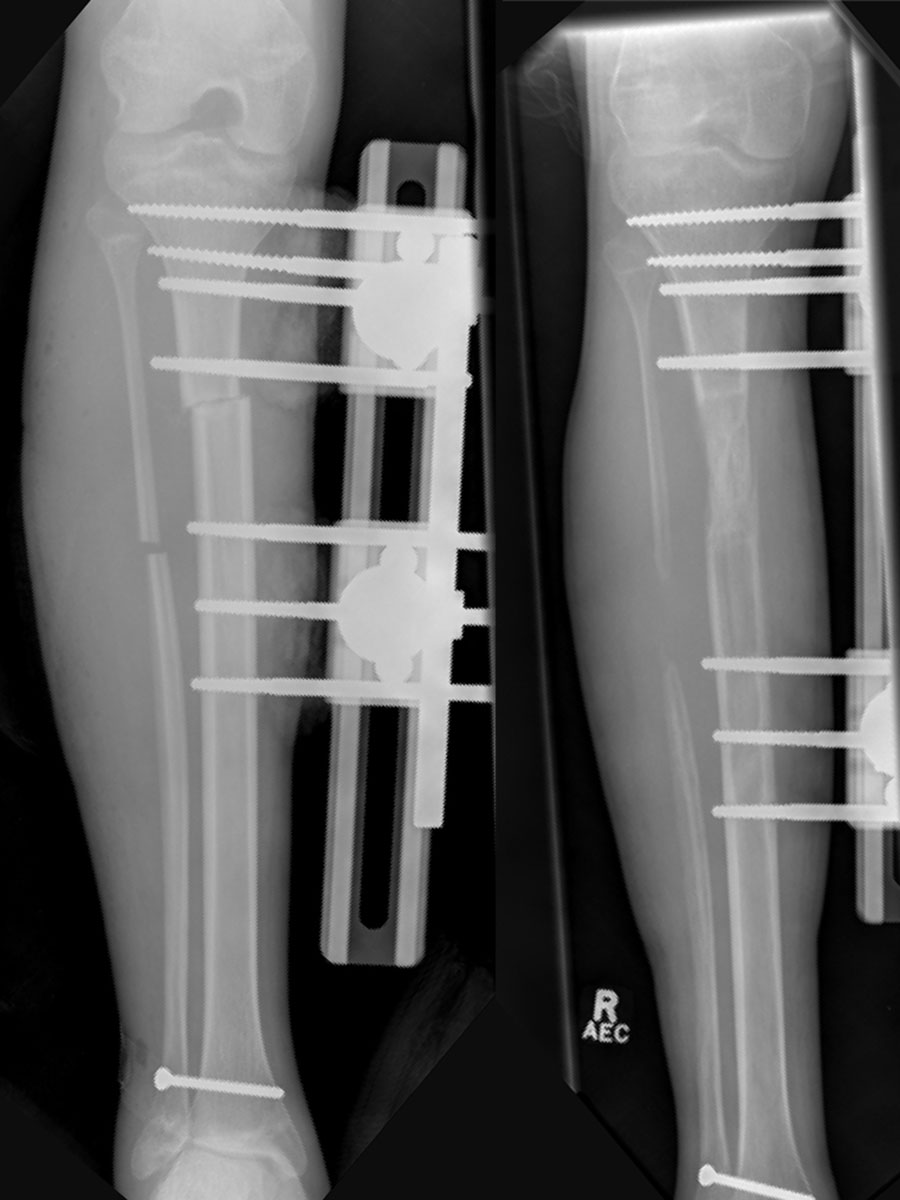
This document focuses on the Ilizarov (pronounced - Ill-is-are-off) method of limb correction. This method takes advantage of the body’s remarkable ability to grow new bone tissue. It involves the surgical application of a circular or rigid straight metal frame called the external fixator. Fixators are attached to each segment of the original bone through pins and wires, which hold each bone segment in place while new tissue is growing and maturing.
A circular or “fine wire” frame as popularised by Dr. Gavriel Ilizarov consists of a combination of pins exiting one side of the bone and wires which pass fully through the bone and are connected to metal rings circling the limb and connected by bars.




A “monolateral” frame uses pins exiting only one side of the bone connected to a bar or adjustment device.
External Fixation Technique
Bone correction is performed by cutting the deformed or angled bone and applying an external frame, using pins or wires passing into bone on each side of the correction site. The correction may be completed at the time of surgery and the frame simply used to stabilise the bone ends whilst they join / unite. In other cases (especially bone lengthening) minor adjustments are made to the frame 4 times per day (by turning nuts or screws) to move the bone ends by approximately 1 mm per day. Such a slow movement “tricks” the body into healing the resultant gap constantly. The new bone that forms in the gap slowly hardens until a time when the frame can be removed. Occasionally internal fixation (plates or rods) may be added to further stabilise the corrected bone.
Team Approach
Stabilisation of a bone or gradual limb deformity correction with an external fixator requires a team approach. Dr. Mackie will provide education, the surgical process and regular follow-up. It is important for a treating general practitioner to be aware of the planned intervention and to engage with a local physiotherapist who will assist with mobility and exercises.
The Patient is the most crucial team member because active participation is valuable to the success of the limb correction process. Patients may be required to assist with fixator adjustments, as instructed. Without a commitment to goals, and providing important feedback along the way, other team members cannot operate as effectively in their roles. It is important for family or close friends to be informed of a proposed frame treatment, as the appearance of an external frame can be a shock to some people.
Phases of Frame Treatment
Some external frames are applied to simply stabilise / support a corrected bone or joint position. Others are applied in a manner that allows the slow correction of the deformity. There are several stages to the Ilizarov process of slowly correcting a deformity.
The initial stage is the principal corrective phase. The second is the consolidation phase.
The corrective phase
This refers to the period of time it takes to “correct the bone or grow the bone (if lengthening is being performed).” This phase begins after Dr. Mackie cuts the bone and attaches the fixator. During this time the patient may have to play a role in making gradual adjustments to the fixator, which moves bone ends or increases the gap between the bone segments, adding “length” to the total limb. Over a period of weeks to months, new bone tissue will grow in the gap, ultimately hardening the area between the segments of the original bone. Occasionally minor adjustments may be made to the frame in brief returns to the operating theatre. When the patient and Dr. Mackie are satisfied with the length and position of the new bone, the consolidation phase begins.
The consolidation phase
During this phase, the bone tissue matures and becomes solid. Patients still have the fixator attached, but will not make adjustments. The consolidation phase is the longest part of the Ilizarov process. It takes twice as long for the bone to harden as it does to lengthen it, so the consolidation phase typically doubles again the time spent in the lengthening or corrective phase.
In preparing for the process it must be noted that patients who undergo lengthening of severe defects may require a frame on their leg for up to 1 year, with most on for 2 – 3 months or more.
Planning for the Journey
The limb correction process takes a great deal of preparation as well as personal commitment. Patients should remain physically active whilst wearing the fixator. It is important to maintain as many daily routines as possible and continue attending school, work, and social activities. This will entail planning. To prepare patients and family for this new lifestyle, quite a few issues need to be considered.
Hospitalisation
The initial hospital stay is generally for around three to four days. This will allow time for postoperative pain to settle down, and time to become familiar with the frame and its management.
Fixator Adjustments
If planned surgery will involve ongoing frame adjustments these will need to be performed by the patient or a family member up to 4 times per day. An early commitment is required to follow a schedule of fixator adjustments, as close as possible to every 6 hours.
Scheduling Considerations
Planning ahead is necessary for the amount of time away from school or work, frequency of office visits, time of year and transportation issues. During the corrective phase of Ilizarov treatments regular consultations (sometimes weekly) will be required to check on the frame stability, to ensure no complications and to check on X-ray monitoring of the bone healing. Range of motion of adjacent joints may be checked to determine if physiotherapy requirements should be altered. Fewer consultation visits will be required during the consolidation phase.
Changes to Normal Activities and Physical Limitations
Some thought needs to be given ahead of time what activities might or might not be able to be accomplished whilst a frame is in position. More time, preparation, energy and rest will be needed to perform daily activities. See the Activities of Daily Living section at the end of this document for more details.
Clothing Adaptations
Loose clothing, which will fit over the fixator will need to be considered and possibly planned-for. See the Clothing Modifications section of this brochure for more information.
Household Furniture and Linens
Furniture and linens can be protected from damage caused by the fixator by wearing a protective covering over the frame or covering any sharp edges. Wrapping the frame with a robust material can be helpful.
Physiotherapy
Within several days of Ilizarov surgery, patients may begin a rehabilitation program designed to improve blood supply to the limb and promote healing. If having a leg lengthened or straightened, it will be necessary to participate in physical therapy in the hospital until able to walk or mobilise with crutches.
A physiotherapist may need to teach patients exercises to help develop sitting and standing balance, stability, and coordination in order to prepare for mobilization and ambulation. A therapist may prepare a home-exercise program designed to maintain the limb’s range of motion and strength. Their objective is to help patients become as independent as possible in personal care and daily activities.
Aerobic activity increases blood flow and strengthens bones. It burns calories, increases resistance to disease and decreases tension. It also releases endorphins – the body’s own pain-control system. An exercise program will depend on the type of injury or deformity sustained and external fixation device in use. To avoid complications, it should be followed with commitment and discipline. Patients may be able to walk or ride a stationary exercise bicycle.
Many patients will be instructed to bear weight on the affected extremity to encourage healing, with the frame providing enough support for some weight bearing (or often full weight bearing) to occur. Whatever the method, exercise is critical for a speedy recovery.
Weight Bearing
Before walking with crutches, it is imperative that patients are fitted properly for them and that they know how to ambulate correctly and safely. Dr. Mackie will plan a weight-bearing status for patients after surgery, which will be partial weight bearing or full weight bearing.
It is possible to practice correct weight bearing status with bathroom scales.
E.g. If an 80 kg man is asked to remain at “50%” weight bearing he will use bathroom scales to get a feel for 40 kg pressure on his leg, subsequently reproducing this feeling when walking.
Crutches and comfort
- Crutches should be custom adjusted to body size by a physiotherapist.
- A thick foam rubber pad on the underarm piece may relieve pressure of the crutch on the upper arm and thoracic cage. But it is important to not place pressure in the axilla (armpit) when using crutches. Weight should be supported on the hand pieces to avoid damage to the nerves under the armpits (brachial plexus nerves), which can cause “crutch paralysis”.
- Crutch walking can take a toll on the hands. Protection of hands from pain and calluses is aided by using hand-piece pads in good condition.
- Crutches should have large rubber suction tips.
- Good balance and erect posture are essential for crutch walking. Learning to balance by standing next to a chair on the unaffected leg can be helpful.
- Wearing well-fitting shoes with firm soles to prevent falls.
- Staying away from wet, slippery surfaces, freshly waxed floors, and rough, uneven surfaces will help prevent falls.
- Going up and down stairs requires both strength and flexibility. Patients should ensure someone is by their side until they have regained strength and mobility.
- To go up and down stairs remember – up with the good leg, down with the affected leg… Or “Good leg up to heaven and bad leg down to hell”.
Frame Adjustment
Adjusting the Fixator at Home
If patients are having a limb slowly lengthened or corrected, they will be required to assist in the process by making fixator adjustments at home. This is usually done every six hours. Dr. Mackie will make sure patients are trained and understand how to make adjustments. They may also receive a specific “turning” schedule at each clinic visit. There may be occasional failure of the mechanics of the fixator. Any broken wires, bent rods or screws that are unable to be turned require a call to Dr. Mackie’s office to arrange assessment.
Frame adjustment usually commences 5 days (children) and up to 10 days (adults) after the initial surgery. The time period allows the body to “start” the healing process, which is utilised by the Ilizarov technique. By performing the adjustments in very small and frequent increments (1/4 mm per turn and 4 turns per day results in 1 mm per day total) pain levels are much reduced (as well as providing a more reliable bone growth). Some frames (Taylor Spatial Frame especially) may only require 1 adjustment per day.
Monolateral frames
Often a single hexagonal screw needs to be turned 4 times per day during the correction phase.
Circular frames
Small nuts on the threaded rods will need to be turned 4 times per day, instructions are provided depending on the frame. Some frames use “clickers” which provide an easier method of turning the nuts.
“Taylor Spatial” frames
These more complex frames have 6 struts with distance markings on each metal strut. A computer printout instructs patients as to the specific mark each strut should be set to for every day of the correction phase.
Nutrition
Attention to nutrition is an important way to assure the speedy healing of new bone as well as keep the rest of the body in good shape for the extra physical and emotional demands. A well- balanced diet with adequate protein, minerals and vitamins is needed for healthy tissue-and-wound healing. Calcium supplements are generally not required if a good diet is maintained. Throughout the process, patients should avoid drinking colas and other drinks, which contain excessive phosphoric acid. They may decrease the amount of calcium the body absorbs.
Stop Smoking
Avoid smoking (even secondary smoke). The nicotine in cigarettes interferes with bone formation and harms the body’s ability to heal. Nicotine patches should not be worn because they can produce the same bad effect.
Coping with Pain
Pain management is essential to well-being and recovery. Pain may decrease a desire and ability to walk and actively participate in physical therapy. Pain also may cause the adoption of protective postures, such as keeping the knee bent or the foot extended, which may lead to joint stiffness and decreased joint mobility. Although the bone transportation itself should not be painful, poor pin care may cause the skin around the pin sites to become taut, causing pain at the level of the skin.
Patient attitude throughout the Ilizarov process is important to its success. This means finding ways to cope with discomfort, pain and frustration, plus the natural ups and downs of emotions during this long process.
Each individual experiences pain differently so it is difficult for medical professionals to discuss norms. (Remember this when talking to other Ilizarov patients, general practitioners and physiotherapists.) During the first few days after surgery, it is likely that patients will feel moderate pain or discomfort. Whilst in hospital pain medication is administered as needed. Pain medicine may be given intravenously for the first couple of days. After discharge from the hospital an over-the-counter pain medication (such as Panadol) may suffice but in some cases a prescription pain killer may be needed. Over-the-counter anti-inflammatory medications (such as Nurofen) should be avoided. These drugs decrease the bone-healing rate by reducing the inflammation that is necessary for the process of bone formation. Pain medicines should be taken before therapy and at bedtime as needed for comfort. Whatever the degree of pain, it should get progressively less bothersome.
Ways to Alleviate Pain
- Continue with exercises. Do not allow the knee or ankle to become stiff.
- Keep the pin sites clean.
- Elevate the affected extremity while at rest, securing position and proper alignment to decrease pain and swelling.
- Take pain medication at least 30 minutes prior to exercise to facilitate easier movement with less discomfort.
- Practice relaxation, distraction and imagery techniques to calm and relax muscles.
- Patients should contact Dr. Mackie or the general practitioner promptly if they experience increased pain, discomfort or swelling unrelieved by rest.
- Know that the discomfort associated with the device is usually mild.
- Anticipate early mobility.
- Keep a good attitude and sense of humour.
- Know that the device is temporary.
- Think about the rewards at the end.
- Actively participate in the care associated with the fixator.
- Normal activities of daily living may be more time consuming. Allow enough time for these activities to avoid frustration. Keep active.
Pin and Wire Site Care
Skin infection is a common problem around pin sites but may be avoided with proper pin care. A major responsibility that patients perform as a team member is making sure the areas of pin sites and wires are cleaned daily.
Patients may not be allowed to shower for approximately five to seven days after placement of the external fixation device. If they have an incision, they may not be able to shower until the stitches or staples are removed. Until patients are able to shower they (or carers) may have to clean the pin sites with cotton swabs and normal saline. During the first few days after the application of the external fixator, expect clear yellow or slightly bloody drainage from the pin sites. To remove this drainage, saturate a cotton swab in normal saline. Start at the pin site and move outward, using a circular motion. Each cotton swab should be used only once and then thrown away. Cotton swabs also may be utilized to remove dried blood and scabs from the pin sites and keep the skin from adhering to the pins. It is important though to be careful not to irritate the skin. Excessive skin motion on the pin may cause infection. If patients have difficulty reaching or seeing all the pin sites, they may ask a family member or friend to help or use a mirror. The above method is one of many ways to care for pins and wires.
Showers
Cleaning the pin sites with an antibacterial liquid soap and water while taking a shower has proven to be a simple and effective pin-care method. As long as there are no open wounds and Dr. Mackie allows it, patients can shower with the external fixator in place. Patients are encouraged to wash the external fixator as well as the leg in the shower using a liquid antibacterial soap, allowing the soap and water to run down the extremity. The limb should not be vigorously scrubbed. The fixator and the extremity should be rinsed and then dried thoroughly. Dry using a hair dryer on cool setting.
For safety purposes patients should consider placing a rubber mat in the tub, using a shower chair, and installing handrails in the shower.
Any activities that involve soaking the external fixator in contaminated water are discouraged.
Monalateral frames and large pin sites
After routine cleaning (saline/swab early and shower later) thin strips of dressing gauze can be cut and applied around the pin sites if required. A long strip of gauze can be bandaged around the pin site to help apply a small amount of pressure to the skin immediately around the pin site. If the skin is clean, no dressings are required.
Fine wire sites
A small “stopper” is often slid down the wire onto a gauze dressing or alcohol wipe cut to fit around the wire.
Pin-Tract Infections
Patients are encouraged to call Dr. Mackie’s rooms if they experience:
- Redness, warmth and swelling from the pin sites. A small amount of redness is normal.
- Extremely tender pin sites.
- Persistent fever of 38 degrees or higher orally.
- Thick, cloudy, white, yellow or green drainage from pin sites.
- (Clear yellow or slightly bloody drainage is normal.)
- Odour at the pin sites.
These are warning signs of infection. The office should be called promptly. Early treatment is mandatory. Oral antibiotics and increased pin-site care may be needed to keep the infection from spreading further. Patients with external frames are generally supplied with “standby” oral antibiotics and if minor pin site infections occur they will be advised to use the 5-day course of the antibiotic. In more severe cases of pin site infection (often associated with loosening of the pin or wire) it may be necessary to return to hospital for a couple of days of intravenous antibiotic. It may even be necessary to take some pins out or exchange them for new pins / wires.
Nerve Problems
The first sign of a nerve problem is called referred pain. This is pain along the distribution area of the nerve that occurs due to stretching or pressure against a nerve. The pain is usually in a location where there are no pin sites (e.g. the top of the foot). The next sign may be increased or decreased feeling in the area of the foot. Any concerns should be reported to Dr. Mackie as soon as possible. They may be symptoms of nerve irritation.
During the corrective phase of limb reconstruction surgery the soft tissues of the limb (nerves, blood vessels, muscles, ligaments) need to stretch in much the same way that bone is being stretched and encouraged to adapt. Progressive irritation of these structures may require a slowing of the correction phase whilst they adapt.
Clothing Modifications
Purpose
- Hide the frame.
- Provide warmth during winter months.
- Provide ventilation during summer months.
- Provide a protective shield, preventing dust, dirt and grime from invading the pin sites.
Clothing for Men and Women
- Snap-on nylon sports pants / tracksuits or shorts may be the most comfortable articles of clothing to wear.
- Some snap all the way up to the waistband making them easy to get on and off.
- Trousers can be altered by cutting the inside and/or outside seams up to the crotch and inserting triangular pieces of fabric.
- Secure the fabric inserts with hooks and loops by sewing machine or by placing buttons.
- Select trousers with many pockets for carrying around small items.
- During the summer months patients may wish to wear shorts or cut off the pant leg above the external fixator.
- For women, loose-fitting dresses, skirts or shirts are preferable.
Shoes
- Wear shoes that are comfortable, protect the toes, allow for balance, support and stability and keep the feet warm.
- Sneakers are recommended.
- If the external fixation device covers a portion of the foot, patients may need to modify shoes.
- If the fixator includes the foot, a foot ring with a rubber sole can be added instead of a shoe.
Underwear
- Must have a wide leg diameter.
- Must be very stretchy.
- Can be split in the seam, and snaps or hooks and loops can be added.
Covers for External Fixators
- Custom covers may be able to be sourced (from plaster / splint suppliers).
- Double-thickness stockingettes can be useful.
- Patients may be creative and make their own cover.
Purpose of Covers
- Provide warmth for comfort and circulation purposes.
- Provide protection from dust, dirt and grime.
- Prevent tears in clothing and sheets.
- Prevent damage to furniture.
General Information
Activities of Daily Living
More time, preparation, energy and rest will be needed to perform activities such as cooking, cleaning, shopping, walking, dressing, bathing and laundry. Patients may need the assistance of significant others to help them through this. After all, they are limited as to what they can do. If patients live alone they should make arrangements for someone to help with these activities. If needed, contact with a social worker or home health nurse to assist with these arrangements may be required.
Positioning the Affected Extremity
Immediately after surgery, the affected extremity should be elevated above the level of the heart until there are no concerns about swelling. To elevate the affected extremity properly, a pillow is placed under the heel of foot so that the knee is extended fully.
To move the affected extremity, the leg external fixator must be moved together as a unit. The amount of assistance needed depends on a patient’s ability to control the leg during the move. It is important not to place hands or lifting pressure under the fracture or bone cut site during movement. Lifting the frame at the same time can support the limb.
Sleeping
The body may require more sleep during the time of external fixation due to increased energy demands in ambulation and other activities.
Sleep is probably limited to one position – often on the back. Elevation of the leg with pillows to secure the position of the extremity can provide comfort.
Patients may consider sleeping with the fixator-frame covered to avoid ripping sheets. Strapping a couple of pillows around the frame may also allow patients to roll in bed without scratching themself or the bed sheets.
Sitting
Patients should walk to the chair with their crutches, turn around slowly and back up to the chair until the back of the unaffected leg touches the seat. Grasping both crutches at the hand pieces using the hand on the unaffected side allows the ability to bend forward slightly while assuming a sitting position. Grasping the seat of the chair with the hand on the affected side, and moving the affected leg forward allows a gradual lowering into the seat.
Standing
A move forward to the edge of the chair allows push off against the seat using the hand on the affected side. Pushing down on the hand pieces of crutched while raising the body to a standing position should simply be the reverse of sitting techniques.
Using the Toilet
- Follow the same steps used in sitting and standing for getting on and off the toilet.
- Consider using an elevated toilet seat.
- For safety purposes consider placing handrails beside the toilet.
After the Fixator is Removed
When Dr. Mackie is satisfied with the strength of the new bone, the fixator will be removed in a same-day or outpatient surgical procedure. Many times a cast will replace the fixator to support the new bone for a few weeks. At first, patients will have certain physical limitations, depending on the bones and specific situation (no high-impact activities such as jumping, skiing or tennis).
The new bone remains weak for some time and is at a much higher risk of breaking over several months (back into a new frame!).
